Schedule a Presentation With Us!
- PapaCarie for Caries Removal
- PerioMonitor Saliva Test
- Woodpecker Laser Smart Blue
- Woodpecker Endodontic
We use cookies!
We use cookies to improve your website experience and analyze traffic. These cookies are necessary for the site to function properly and help us understand how you use it. The information collected remains anonymous and is used for analysis purposes only. By continuing to browse our site, you accept the use of these cookies. If you do not want your data to be used in this way, please click decline. You can read our document on the potection of personal information (Law 25) here
High molecular weight hyaluronic acid (HA) is a natural physiological constituent of connective tissue.
It plays a critical role in the collagen-making process. Made up mostly of collagen, it is one of the major
components of the human body. HA is the most abundant high molecular weight glycosaminoglycan of healthy
soft periodontal tissues.4 It is active in tissue regeneration and influences the migration of fibroblasts and
fibrinogenesis, thus making the healing of tissue easier. It performs 3 synergistic effects: anti-inflammatory,
accelerates the healing process and provides a protective barrier.
Contributing to the barrier function and tensile strength of the periodontal ligament, HA is essential for healthy
gingival tissues. In the initial stage of inflammation and periodontal disease, tissue’s requirement for HA
increases by 200%, demonstrating its central role in regulating cell turnover and optimizing tissue regeneration.
When lacking HA, healing will be delayed and inflammation will continue
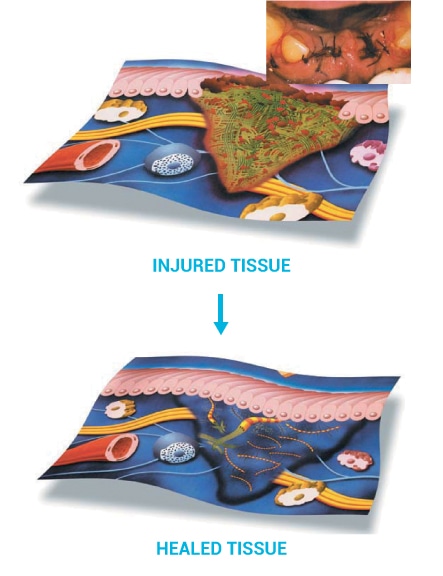
1. ANTI-INFLAMMATORY PHASE
• Enhanced inflammatory cell and extracellular matrix cell infiltration into the inflamed site
• Elevation of pro-inflammatory cytokine production by damaged tissue
• Stabilizes granulation tissue matrix
• Scavenges free radicals such as superoxide (O2) and hydroxyl radical (OH)
• Inhibition of inflammatory cell-derived proteinases
2. GRANULATION PHASE
• Increases organisation of the granulation tissue matrix
• Increases extracellular matrix cell proliferation
• Increases inflammatory cell and extracellular matrix cell migration
• Increases blood vessel formation (angiogenesis)
3. REPARATIVE PHASE
• Increased fibroblasts and collagen
• Fibrous tissue formation
• Migration and proliferation of keratinocytes
• Rapid epithelialisation and wound healing